By selecting the Yes option, leaving Amgen.eu option you understand that you are leaving the corporate page of Amgen Europe and that you will be redirected to another Internet site belonging to third parties, for whose content or opinions Amgen Europe is not responsible and makes no representations regarding such content or its accuracy. By selecting this option and accessing linked third party sites, you understand that you do so at your own risk.
The website to which you will be redirected may be designed exclusively for residents of a particular country or countries, as advertised on that website. As a consequence, the website to which you will be directed may contain information on pharmaceutical products or indications that are not approved in Europe. If You reside in a country other than the one to which such website is directed, please contact your local Amgen affiliate for the correct information on products in your country of residence.
Why PROCYSBI
PROCYSBI® is designed to work over 12 hours. PROCYSBI (cysteamine bitartrate) delayed-release capsules or delayed-release oral granules should be taken every 12 hours at the same time every day as prescribed by the doctor. For example, a person might take PROCYSBI at 8:00 a.m. and again at 8:00 p.m.
PROCYSBI® (cysteamine bitartrate) delayed-release capsules and delayed-release oral granules are the first and only cysteamine therapies with 12-hour dosing approved for the management of nephropathic cystinosis in adults and children at least one year old.
PROCYSBI helps reduce cystine levels with 2 doses in 24 hours, taken every 12 hours at the same time every day, allowing patients and caregivers to choose consistent times that work for them. For example, a person might take PROCYSBI at 8:00 a.m. and again at 8:00 p.m. every day. This means people with cystinosis can make routines that fit their schedules.


In clinical trials with people with nephropathic cystinosis who took PROCYSBI every 12 hours as directed:
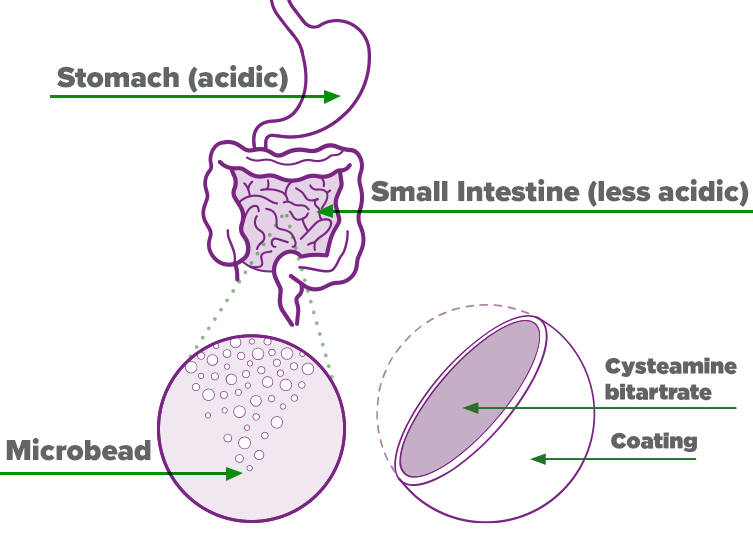
PROCYSBI is a delayed-release formulation of cysteamine bitartrate that was designed to release in the small intestine instead of the stomach. A coating on the microbeads helps control how and where the medicine is released in the body. The coating does not break down in acidic environments, such as the stomach. Instead it breaks down in less acidic environments like the small intestine.
Hi, I’m Hannah and I’m currently a college student studying voice. I love music and being outdoors, and I’ve also been riding dirt bikes since I was 7!
I was diagnosed with nephropathic cystinosis when I was 15 months old and have been managing my condition from a young age. I think the most difficult thing to understand about this condition is the extent of damage that a buildup of cystine can cause throughout the body.
Nephropathic cystinosis can be difficult to explain, so let’s take a closer look inside the body.
Cystinosis is a rare, genetic condition that causes an amino acid called cystine to build up and form crystals throughout the body.
Amino acids like cystine are the building blocks that make up protein.
Nephropathic cystinosis is the most common form, seen in about 95% of cases. It causes severe damage to the kidneys and other organs in the body.
People with nephropathic cystinosis have cells that are unable to remove cystine like they normally should. The cystine builds up and forms crystals within cells, affecting every organ of the body.
This can lead to damage throughout the body, causing kidney disease, problems with the bones, sensitivity to light, thyroid problems, diabetes, kidney failure, weak muscles, and difficulty breathing.
Cystine starts to build up in the cells of the kidney before the child is born, causing symptoms of kidney disease by 6 months of age. This eventually leads to kidney failure in patients with nephropathic cystinosis.
Although existing organ damage cannot be reversed, disease progression can be slowed with cystine-depleting therapy, or CDT.
CDT is currently the only treatment available that can remove cystine from the body. When taken correctly, CDT lowers the amount of cystine in the cells.
PROCYSBI (cysteamine bitartrate) delayed-release capsules and delayed-release oral granules is the only CDT with 12-hour dosing which means you take it two times a day, every 12 hours.
For example, you might take PROCYSBI at 8:00 a.m. and again at 8:00 p.m. each day.
PROCYSBI works to control cystine levels continuously over 12 hours.
PROCYSBI granules, also called microbeads, are composed of medicine surrounded by a protective coating.
The coated microbeads allow the medicine to pass through the acidic stomach and into the less acidic small intestine without dissolving.
Once in the small intestine, the coating begins to dissolve and the microbeads release medicine gradually, which allows PROCYSBI to control cystine continuously over 12 hours. In order for PROCYSBI to work the way it should, it must release only in the small intestine. So it’s important to take PROCYSBI exactly as directed to prevent the medicine from being released into the stomach instead of the small intestine. This means the inside of your stomach should be acidic.
Certain foods and drinks can lower the amount of acid in your stomach, causing the medicine to be released before it reaches the small intestine. This can cause stomach pain, nausea, and vomiting. This can also cause PROCYSBI to act differently in the body than it should.
This is why you should take PROCYSBI capsules with drinks like water or fruit juice (except grapefruit juice), and mix PROCYSBI granules with foods like applesauce or berry jelly, all of which are acidic, to keep the acid in your stomach higher.
It's important to tell your doctor about all the medicines you take. Certain medicines, like antacids containing bicarbonate or carbonate, can lower levels of acid in the stomach.
This may cause PROCYSBI to release too soon into the stomach. You should take PROCYSBI at least 1 hour before or after taking medicines that contain bicarbonate or carbonate. Talk to your doctor or pharmacist before you begin taking a new medicine.
Don't eat fatty foods right before or after taking PROCYSBI because fat in the small intestine will reduce the absorption of PROCYSBI.
Do not drink alcohol while taking PROCYSBI. Alcohol may cause PROCYSBI to be released too quickly, which affects how well PROCYSBI works and may cause serious side effects.
Your doctor should order a blood test to check the amount of cystine in your blood cells. This helps the doctor decide if you need a change in your dose of PROCYSBI. It’s recommended that your cystine levels be checked at least twice a year. Work with your doctor to create a schedule that’s right for you.
It’s important to remember that nephropathic cystinosis is a lifelong disease that causes damage over time without proper treatment.
This is why it’s important to take PROCYSBI as prescribed, the same way and at the same time every day to help control your cystine levels. Because, without regular treatment, cystine will build up and cause organ damage throughout the body even if you may look and feel fine.
We all have busy lives, and it can be hard to balance your treatments with your personal life, especially if you’re feeling fine! But I know it’s important, so I create a schedule that works for me. I set up my medicine for the week on Saturday in separate containers. I have timers on my nightstand and on my phone that alarm 5 minutes before and after it’s time to take my PROCYSBI. I set 3-4 alarms so I won’t forget! I always take my PROCYSBI capsules the same way, with water, at the same times every day. My doctor helped me to come up with a meal plan that works best for me, too.
Taking charge of my cystinosis at a young age has definitely helped me to become more responsible and independent. But I know there’s always a group of people around me who support me. If you’re just starting PROCYSBI, or are having trouble keeping up with your doses, talk to your doctor for more information and to create a routine that works for you. And remember, cystinosis doesn’t define you, you define cystinosis!
PROCYSBI (cysteamine bitartrate) delayed-release capsules is a prescription medicine used to treat a medical condition called nephropathic cystinosis in adults and children 1 year of age and older. It is not known if PROCYSBI is safe and effective in children under 1 year of age.
PROCYSBI can cause serious side effects, including:
Do not take PROCYSBI if you are allergic to penicillamine or cysteamine.
Tell your doctor if you have any other medical conditions, including if you:
See “What is the most important information I should know about PROCYSBI?”
The most common side effects of PROCYSBI include: vomiting, nausea, stomach (abdominal) pain, breath odor, diarrhea, skin odor, tiredness, skin rash, headache, problems with body salts or electrolytes.
These are not all of the possible side effects of PROCYSBI. Call your doctor for medical information about side effects.
You are encouraged to report all the possible side effects of prescription drugs to the FDA. Visit http://www.fda.gov/medwatch to call 1-800-FDA-1088.
Find out more about cystinosis, the damage it can cause, and how PROCYSBI may help.
PROCYSBI passes through the stomach before it reaches the small intestine. Once in the small intestine, the medicine in PROCYSBI is gradually released over 12 hours—just long enough for the next dose of PROCYSBI to reach the small intestine. This gradual release of cysteamine ensures continuous dosing.
When acid levels in the stomach are higher, the microbead coating works as it should and doesn’t release the medicine until it reaches the small intestine. What a person eats and drinks can affect acid levels. If acid levels are too low, it can result in the medicine releasing too soon (in the stomach).
Do not drink alcohol while taking PROCYSBI. Drinking alcohol while taking PROCYSBI may change how PROCYSBI works and may cause an increase in the amount of PROCYSBI in the blood that may cause serious side effects.
When taking PROCYSBI as directed, continuous cystine control may be achieved. Talk to your doctor about how to take PROCYSBI with foods that have an appropriate level of acidity to ensure that it doesn’t dissolve in the stomach.
Tell your doctor right away if you develop any of the following symptoms while taking PROCYSBI: headache, buzzing or "whooshing" sound in the ear, dizziness, nausea, double vision, blurry vision, loss of vision, pain behind the eye, or pain with eye movement.
PROCYSBI (cysteamine bitartrate) delayed-release capsules and delayed-release oral granules is a prescription medicine used to treat nephropathic cystinosis in adults and children 1 year of age and older. It is not known if PROCYSBI is safe and effective in children under 1 year of age.
Do not take PROCYSBI if you are allergic to penicillamine or cysteamine.
Before taking PROCYSBI, tell your doctor about all your medical conditions, including if you:
Tell your doctor about all the medicines you take, including prescription and over the counter medicines, vitamins, dietary and herbal supplements. Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
PROCYSBI can cause serious side effects, including:
The most common side effects of PROCYSBI include: vomiting, nausea, stomach (abdominal) pain, pink eye, diarrhea, cold, tiredness, flu, headache, problems with body salts or electrolytes, infection of ear, nose or throat, joint pain.
These are not all the possible side effects of PROCYSBI. Call your doctor for medical information about side effects. You may report side effects to FDA at 1-800-FDA-1088.
For additional important safety information, click here for the Patient Package Insert and discuss with your doctor.